Breeder/Exhibitor Ed, Health
What is dilated Cardiomyopathy (DCM)? Dilated cardiomyopathy is an acquired disease that is characterized by a markedly enlarged and weakened heart muscle. In the Doberman it affects mainly the left ventricle and left atrium. It results in electrical abnormalities (irregular or abnormal or premature beats). These electrical abnormalities may result in sudden death (described below) as the very first clue of a problem in your dog. Most dogs experience symptoms of pulmonary edema with respiratory distress. DCM is observed in dogs, cats and humans, as well as a number of other species. Dilated cardiomyopathy is always rapidly fatal in Dobermans.
What breeds of dogs are affected with DCM?
DCM is more common in large breed dogs than in small breed dogs. However we have observed DCM in a large variety of small breed dogs. In a study that attempted to enrol any dog with DCM throughout North America, more Dobermans were enrolled than all other breeds combined.
The following chart provides a listing of the breeds enrolled with DCM at that time:
- Cocker Spaniels 4.1%
- Doberman Pinschers 55.7%
- German Shepherds 5.7%
- Great Danes 7.1%
- Irish Wolfhounds 4.3%
- Labrador Retrievers 5.7%
- Old English Sheepdogs 4.3%
- Terriers 1.4%
- Others 11.4%
As one can see more Dobermans were enrolled than all other breeds of dogs combined. I take this to suggest that there is more DCM in this breed than in all other breeds combined and to also mean that there must be a genetic predisposition for DCM in the Doberman.
What is the cause of DCM?
Most cases of DCM are called idiopathic. This means we do not know the cause of the DCM. Some cases of DCM are due to heart rate abnormalities such as when the heart rate is too high. Other cases are due to a nutritional disorder such as a deficiency of taurine. This does not appear to be the case in the Doberman. In people, viruses are suspected to cause some cases of DCM. We looked for evidence of parvo virus in Dobermans with DCM and could not find evidence of this virus.
In people, an immune mediated disorder (somewhat like rheumatoid arthritis) has been speculated to cause DCM. We looked for evidence of an immune disorder in Dobermans with DCM and could not find evidence of this process at work. In people, about 30% of cases of DCM are familial. Sounds somewhat similar for the Doberman.
What is the incidence of DCM in the Doberman Pinscher?
Work performed at the University of Guelph has demonstrated that about 50% of all symptom free Dobermans in our area will develop/acquire DCM. Reports out of the University of Georgia indicate that about 50% of symptom free Dobermans studied there will go onto develop/manifest DCM.
Does the incidence of DCM in the Doberman Pinscher vary with the sex of the dog? Males are more affected than females. Our work suggests that about 60% of symptom free male Dobermans in our area will develop/acquire DCM. Also about 40% of symptom free female Dobermans will go onto develop DCM.
Does the incidence of DCM vary with the coat color of the Doberman Pinscher? Our work indicates that red and rust Dobermans are equally affected compared with black and rust Dobermans. The other two phenotypes, blue and Isabella (fawn), are too infrequently studied to be able to address the incidence in these groups.
At what age do Dobermans get DCM?
The average age that Dobermans develop symptoms of DCM is 7.5 years of age. However 25% of our dogs developed symptoms of DCM over 10 years of age.
What are the usual symptoms of DCM in the Doberman?
Dobermans may manifest one of two common symptoms related to DCM. Respiratory distress, usually noted as a cough, wheeze, or labored breathing, is the most common symptom of DCM. The next common symptom is called sudden death. In sudden death owners usually observe that their dog was running in the yard then fell over and died. They are dead within a couple minutes. One third of all Dobermans destined to develop/acquire DCM will experience sudden death as the first symptom of their disease. A few dogs are noted to demonstrate a loss of stamina (also called exercise intolerance) as the main sign of DCM.
What is sudden death in Doberman Pinschers?
Sudden death is a common symptom of DCM in otherwise symptom free Doberman Pinschers. We presume that the dog developed a severe rhythm disturbance (ventricular fibrillation) which resulted in essentially no output from the heart and subsequent death.
Sudden death is death that occurred within one hour of what appeared to be a stable individual. Essentially sudden death represents unexpected death. Sudden death is the first and thus only symptom of DCM in one third of all Dobermans destined to develop/acquire DCM. The presence of frequent PVCs (or VPCs) likely identifies dogs at risk for sudden death. We believe that a Holter exam (a 24-hour ECG; it collects about 130,000 beats in 24 hours) is the best test one can perform to check for the risk of developing sudden death in a symptom free Doberman.
What is the prognosis for Dobermans with DCM?
The prognosis for Dobermans with DCM is much worse than for other breeds of dogs with DCM. It is reported that the average survival for Dobermans with congestive heart failure due to DCM is 90 days with the best of current medication (as of May 2000; whereas the average survival for non-Dobermans with congestive heart failure due to DCM is 280 days with the best of current medication (as of May 2000).
What is occult DCM?
Occult DCM refers to dogs that have some abnormality with their heart but
demonstrate no symptoms for their owners. Thus the owners are unaware that within the chest a problem is stirring. Only when the cardiac disorder
becomes more severe do dogs manifest symptoms of heart failure. The current criteria we have observed and are using to indicate that a dog is in the occult stage of DCM is evidence of heart enlargement on cardiac ultrasound (echocardiography) or the presence of irregularities in the heart rhythm (finding PVCs on the ECG). All dogs that are destined to develop DCM and congestive heart failure manifest a time chart (or time line) that goes through three stages. The first stage is characterized by the absence of symptoms of heart disease and a normal heart on all clinical tests (including echocardiography, ECG, Holter, and other tests). The second stage, we are calling occult DCM, is characterized by the absence of symptoms of heart disease but evidence of DCM based on clinical tests (especially echocardiography, ECG, or Holter). The third stage, we are calling overt DCM, is characterized by symptoms of heart failure and evidence of DCM based on clinical tests. As of today (May 2000), using markers of occult DCM developed at the University of Guelph, the average duration of this occult DCM stage is about 2 years. We have also shown that the introduction of an angiotensin converting enzyme inhibitor during this occult stage of DCM will delay the progression to the third and final stage of DCM by at least an additional 1 year above and beyond the average two years for Dobermans not treated.
What is a Holter monitor?
A Holter monitor or recording (also called ambulatory electrocardiography) is a recorder (usually a cassette recorder although some now hold and use a small computer chip) that is placed or attached to the chest of the dog with bandage material. It enables one to collect all the heart beats a dog (or person) will produce in 2
4 hours. Also importantly this is done in the environment of the dog, that is in the dog’s household and while the dog is running at the park, etc. Hence we are able to relate any abnormalities to the activity of the dog should there be a relationship.
What does a Holter examination tell us?
A Holter exam is used to tell us:
If an apparently normal Doberman has reached the second stage of DCM (also called occult DCM). If this is the case it means the dog should be started on medication to delay the progression to the third and final stage of DCM. That the dog is at risk for developing sudden death.
As of today (May 2000), the Holter exam provides us with 24 hours of ECG (this will collect about 130,000 heart beats). This test will allow us to determine the presence and number and complexity of abnormal heart beats (called PVCs) (potentially a very strong marker for dogs in stage two of DCM and destined to die of DCM if the frequency and or complexity of PVCs is substantial). In addition, this test will allow us to measure Heart Rate Variability (a measure of the balance of adrenalines in the body and a risk marker for people and presumably dogs at risk for sudden death). Most Holter exams are analyzed by human laboratories. As a result the data usually carries many errors, due to the differences between dogs and people. Overall, it should be able to tell you if PVCs were present or not but an accurate count is usually not available. I recommend you have your Holter exam analyzed by a veterinary institution. At the University of Guelph we employ a rigorous quality control program on all analyses such that each 24-hour exam requires from 2 to 5 hours of work to correct/review the automated analysis by the analyzer to ensure an accurate report.
What are PVCs or VPCs?
PVCs refer to premature ventricular contractions. VPCs refer to ventricular premature contractions. These are identical; two short forms for the same thing. They can only be identified on the ECG whether it is a short study (up to 3 minutes) or a 24-hour study (Holter exam). PVCs occur in the second and third stages of DCM. PVCs are of most interest to us in symptom free Dobermans because their presence serves as a marker for Dobermans in the second stage of DCM (occult DCM) if they are sufficiently frequent. We used to believe that all symptom free Dobermans with as few as 1 VPC on a 3 to 6-minute ECG identified dogs in stage two of DCM. However, we have observed a number of dogs with very few VPCs on a routine ECG that over many years never went on to develop DCM. Thus, dogs with very few VPCs may or may not be destined to acquire DCM.
Is a routine ECG better than a Holter Exam?
Both the routine ECG (a 3 to 6-minute exam) and the Holter are used to determine if PVCs are present so as to ascertain if that symptom free Doberman has occult DCM. PVCs can occur very intermittently. We have observed one dog that had 2 PVCs in a one hour period and had 2500 PVCs in the subsequent hour. So you can see how easy it could have been to miss the fact that lots of PVCs are occurring in that individual. It has been clearly demonstrated in people that at least 8 hours of Holter should be collected. So the answer to the question is without a doubt a Holter exam is profoundly superior to a routine ECG. The only reason to use a routine ECG instead of a Holter exam is for those people that cannot have one performed on their Doberman. In the past it was difficult to obtain a Holter exam on Dobermans in certain areas of the country. With the current Holter Project at the University of Guelph, your dog can have a Holter performed as long as you have a postal address that directs the location for us to send the recorder. You might have thought that a routine ECG might be substantially cheaper than a Holter. The cost of participating in the Holter Project at the University of Guelph is only $60. The usual cost for this type of examination through your veterinarian is more than $250.
Is a Holter study better than an ultrasound or chest x-ray?
I believe a Holter exam and a cardiac ultrasound (echocardiogram) are vastly superior to a routine chest x-ray to screen symptom free Dobermans for occult DCM. We have not tested whether on average the Holter exam is superior to the echocardiogram in screening symptom free Dobermans for occult DCM. Clearly we see some dogs that show enlargement before irregular beats (PVCs) and so echocardiography would be the better test in these cases. However, on average it is my belief that the Holter examination will identify dogs that have reached the second stage of DCM (occult DCM) earlier than the echocardiogram. Recognize that the earlier a Doberman can be recognized as in the occult stage of DCM the sooner therapies can be started to help him/her. Note that one test identifies abnormalities of heart size and strength (the echocardiogram) and the other identifies electrical abnormalities (presence of PVCs) (the Holter exam). Hence, the best scenario is to do both tests. Today the Holter examination is much cheaper (if performed as part of the Holter Project research performed at the University of Guelph, only $60).
Should your Doberman have a Holter examination?
If you want to have an opportunity to identify the potential for your symptom
free Doberman to develop DCM, then you should have a Holter exam performed. If you want the chance to delay DCM by starting medication as soon as necessary, then you should have a Holter exam performed. If you participate in the Holter Project at the University of Guelph you are also given an opportunity to participate in a treatment trial that offers the potential for your dog to receive the very latest drugs. If you want to be part of an effort to both help your Doberman and help all Dobermans, then you should have a Holter exam performed and have it performed by the Holter Project of the University of Guelph. If you want to check your Doberman at your convenience and in your home, then you should have a Holter exam performed and have it performed by the Holter project of the University of Guelph. If you live somewhat remote from a cardiologist that can perform a cardiac ultrasound examination, then a Holter exam is much easier to perform and much cheaper. As long as you have a postal address, anyone with a symptom free Doberman anywhere in the world can participate in the Holter Project research performed at the University of Guelph, only $60.
Please see more information about this Holter Project at the University of Guelph. This project will Holter your symptom free Doberman once yearly.
Who should participate in a research project involving Doberman Heart Disease?
All Doberman fanciers should participate. “If we don’t care to help make life better for our breed then who should.” Participating in any prospective project gives you a chance to assess the status of your dog and the greatest chance to extend both the length and quality of life of your dog. In addition, you are giving something back to the breed by supporting an effort to extend the life of all Dobes. Please see more information about this Holter Project at the University of Guelph.
What do you as an owner get out of having your dog enrolled into a heart study? The Holter Study?
You get the opportunity to find out that your dog has stage two DCM (occult DCM) before you would ever know your dog has heart disease. This way you have a chance to extend the length of quality life for your dog with early treatment. Your also have a chance to participate in a large effort to find better ways to diagnose and treat Dobermans with occult DCM and overt DCM (congestive
heart failure due to DCM).
What can you do as a Doberman fancier to help reduce heart disease in our breed?
Enrol your Doberman in a prospective study. Encourage other Doberman fanciers to participate in heart disease research. And finally, participate in efforts to raise funds to further efforts to reduce the significance of heart disease in the Doberman breed.
What work is being done at the University of Guelph with respect to heart disease research in the Doberman Pinscher?
CURRENT WORK
THE WELL DOBERMAN PROJECT – This work began 11 years ago. We are studying the natural history of DCM in the Doberman breed. We have been and are continuing to ask the owners of symptom free Dobermans to allow us the opportunity to examine their dogs once yearly. Each examination consists of a physical exam, ECG, and cardiac ultrasound exam. We have examined over 800 dogs in this time period. The objectives of this work have been to:
- Determine the incidence of DCM in the Doberman breed
- Determine if there is a gender difference in the incidence of DCM in the Doberman breed
- Determine if there is a coat color difference in the incidence of DCM in the Doberman breed
- Identify markers of occult DCM
- Identify therapies to delay the development of congestive heart failure in dogs with occult DCM
THE CONGESTIVE HEART FAILURE DOBERMAN PROJECT – This work has also been in progress for the past 11 years. We are studying the ability of newer therapeutic measures to extend the length and quality of life for Dobermans in congestive heart failure (stage 3 DCM).
THE HOLTER PROJECT – This work has been underway for the past 6 months. The objectives of this work are to:
- Determine the incidence of DCM in Dobermans in various regions of the world.
- Identify markers of occult DCM in symptom free Dobermans
- Identify markers for sudden death in symptom free Dobermans
- Identify newer drugs to reduce the incidence of sudden death in symptom free Dobermans
- Identify newer drugs to delay the progression of occult DCM to overt DCM
(congestive heart failure).
What are some of our future plans with respect to research into DCM of Doberman Pinschers?
- To study the role of a new beta blocker, carvedilol, in Dobermans with occult DCM, to delay the progression to overt DCM. To date we have enrolled 15 Doberman Pinschers with occult DCM into this project.
- To study the ability of pimobendan in Dobermans with overt DC (congestive
heart failure) to extend survival and improve the quality of life. To date we have enrolled 3 Doberman Pinschers with congestive heart failure due to DCM into this project.
- To expand the Holter project via increased enrolment and begin the study of new antiarrhythmic agents to prevent / delay sudden death. Between July 2000 and July 2001 we are hoping to enrol 1000 symptom free Dobermans from around the world.
- We have made contact with a molecular biologist that has found the gene responsible for numerous disorders in people. He is an investigator at the Ottawa Heart Institute.
- We have begun discussions with a view to having his group find the genes responsible for DCM in Dobermans. We will know in the next month if his group will work with tissue samples from our dogs to find the culprit genes.
- We will shortly examine the use of measures of diastolic function (measures of the ability of the heart to relax) to identify symptom free Dobermans as occult DCM at an earlier time than is currently possible.
- We will shortly examine the ability of a blood test, level of big endothelin, to predict dogs with occult DCM.
- We will shortly examine the ability of a blood test, level of big endothelin, to predict the length of survival for dogs with overt DCM.
- Work with investigators at the Toronto General Hospital to determine the role of a nutritional cocktail supplement to protect Dobermans in congestive heart failure.
- To date there are more than 10 drugs worthy of studying in Dobermans with congestive heart failure with a view to determining if they can reduce mortality.
- To date there are more than 8 drugs worthy of studying in Dobermans with occult DCM with a view to determining if they can delay the progression to overt DCM (stage 3 DCM).
- List some of the projects we have previously undertaken in the area of DCM of Doberman Pinschers.
- We studied the role of Enalapril to improve survival in Dobermans with congestive heart failure.
- We studied the role of a neuroendopeptidase inhibitor (increase the
availability of ANP) to improve survival in Dobermans with congestive heart failure.
- We studied the role of pacemaker therapy (VDD pacing) to improve survival in Dobermans with congestive heart failure.
- We studied the role of heart rate variability to identify dogs with occult DCM.
- We studied the role of stressing the heart with dobutamine to identify dogs with occult DCM.
- We studied the role of the plasma norepinepherine response to treadmill exercise to identify dogs with occult DCM.
- We studied the levels of myocardial myoglobin in Dobermans with occult DCM, overt DCM and normal Dobermans.
- We began a study of the utility of the Batista Procedure (partial left
ventriculectomy) in the treatment of congestive heart failure due to DCM in Doberman Pinschers.
- We studied the role of parvo virus infection as a cause for DCM in Doberman Pinschers.
- We studied the role of antibodies directed against the heart as a cause for DCM in Doberman Pinschers.
- We collaborated with Iowa State University to determine the role of
mitochondrial genetic material as a cause for DCM in Doberman Pinschers.
- We collaborated with Texas A&M University to determine the role of the dystrophin gene in the cause of DCM in Doberman Pinschers.
- We collaborated with Texas A&M University in examining pedigrees of affected Doberman Pinschers to determine the mode of inheritance of DCM in this breed.
How is DCM diagnosed in Doberman Pinschers?
OVERT DCM (DOGS WITH CONGESTIVE HEART FAILURE DUE TO DCM):
The diagnosis of DCM is relatively easy in these dogs. These are dogs that present with respiratory distress symptoms. Physical examination reveals:
- A heart murmur in 100% of dogs
- An S3 gallop in most dogs
- Irregular beats in most dogs
- An ECG reveals:
- A normal sinus rhythm in most dogs
- A few intermittent PVCs in most dogs
- Atrial fibrillation in 25% of dogs
Thoracic radiographs reveal:
- Generalized heart enlargement especially of the left ventricle and left atrium in all dogs Pulmonary edema in all dogs
Cardiac Ultrasound reveals:
- Dilation of the left ventricle and left atrium
- A very weak left ventricle
Mitral valve insufficiency OCCULT DCM:
- The diagnosis of occult DCM can be difficult. These dogs are free of symptoms of heart disease, that is the owners believe their dogs are normal. The ideal tools to identify these dogs are cardiac ultrasound, routine ECG, and Holter monitoring.
Cardiac Ultrasound reveals:
- Left ventricular enlargement: in diastole > 49 mm, or in systole > 42 mm.
Note that these measurements can vary tremendously depending
on the experience of the technician that generates this data. Routine ECG is a 3 to 6-minute rhythm trace. This reveals:
- At least 1 PVC/min. in most dogs.
24-hour Holter reveals:
- At this time we are uncertain as to the threshold of the frequency of PVCs that indicates dogs in the occult stage of DCM. Our present work with the Holter Project at the University of Guelph will shortly establish the thresholds indicating dogs affected with occult DCM. As of today, we believe a level of > 50 PVCs /hour indicates Dobermans affected with occult DCM.
- Other issues about PVCs such as degree of complexity (PVCs occurring as doublets and triplets, or runs of non sustained ventricular tachycardia) will undoubtedly be found to identify dogs with occult DCM. Our present work with the Holter Project at the University of Guelph will shortly establish the thresholds indicating dogs affected with occult DCM.
How should DCM be treated in Doberman Pinschers?
OCCULT DCM:
Angiotensin converting enzyme inhibitors have been demonstrated to retard the progression to overt DCM. This effect has been much more dramatic in male Dobermans compared with female Dobermans. We are currently working with a new beta blocker, carvedilol, to determine if it can confer additional protection beyond that provided by angiotensin converting enzyme inhibitors. In the near future we anticipate assessing many more agents.
OCCULT DCM WITH LOTS OF PVCs:
PVCs are a common part of DCM in both the occult stage and overt stage. I assess the presence of these as more a sign of occult DCM as opposed to a sign of risk for sudden death. In the near future we hope to describe criteria concerning the nature of the PVCs (and not just their presence) that indicate a real risk for sudden death and not just that occult DCM is present. Once this has been determined, we will be assessing a range of drugs to determine their ability to reduce the risk of sudden death. Today (May 2000), we have been using sotalol to attempt to protect these dogs from sudden death, if we suspect (but unproven) that they are at an increased risk for sudden death.
CONGESTIVE HEART FAILURE WITH DCM:
Today (May 2000), we administer angiotensin converting enzyme inhibitors and diuretics. The highest recommended dose of the angiotensin converting enzyme inhibitor appears to be the best dose.
I am continually searching for the least dose of the diuretic that maintains ease of breathing. The lesser the dose we can use the better in the long run for the dog.
I don’t use digoxin. It is associated with a lot of toxicity and unproven efficacy.
No other drugs are of proven benefit in the dog. However, we are learning to use the following agents:
- Beta blockers, especially carvedilol. Carvedilol is proven to help people with overt DCM. This agent can initially and immediately make the dog worse. Hence, it appears we need to start the dog on a very low dose and increase it slowly. Also it may be best to start this agent after pulmonary edema has been corrected.
- Spironolactone. This agent is more than a diuretic, in fact I find it is too weak a diuretic to be useful as such. However it’s other properties as an agent that blocks the hormone aldosterone appear to be responsible for its benefits in people with heart failure. We are only now learning how to use this agent.
A vital part of the treatment of this disease is the follow-up. I recommend the first recheck occur on 3 to 5 days after first exam. The objective here is to attempt to reduce the dose of diuretic required. I routinely perform a lateral chest radiograph and a serum assessment of kidney function. I also check the heart rhythm for frequency of PVCs or atrial fibrillation. The next checkup occurs about 1 week after first examination, then at 2 weeks, 4 weeks, and then once monthly. The objective is always the same:
- To attempt to reduce the dose of diuretic. As the disease progresses the need for diuretic increases. I check a lateral chest x-ray and serum kidney test to help me decide to reduce the diuretic dose.
- To assess cardiac rhythm
ATRIAL FIBRILLATION AND CONGESTIVE HEART FAILURE WITH DCM:
In addition to the drugs described above, dogs with atrial fibrillation need to receive drugs with the objective of reducing the heart rate. Many Dobermans with atrial fibrillation have heart rates over 200 beats per minute. Our goal is to reduce the heart rate to about 160 beats per minute.
Drugs to accomplish this are:
Beta blockers:
- Atenolol
- Carvedilol
- Sotalol
Calcium channel blockers:
- Diltiazem. As of today (May 2000), this may be our best agent to slow the heart rate.
- Digoxin. This drug will probably not be effective if the heart rate is over 200 beats per minute before therapy. Hence, additional agents will likely be needed.
A vital part of the treatment of this disease is the follow-up just like above. In addition to the issues described above, the rechecks also focus on checking the heart rate with a view to determining if we have achieved the target heart rate. Some nervous dogs may be better assessed with a Holter exam, which will give us the heart rate at home and the trends in the rate throughout the day.
Is there anything I can do to prevent my Dobe from developing DCM?
Absolutely nothing. About 50% of all Dobermans in North America can be expected to develop/acquire DCM. The most anyone can do is to enrol their Doberman in a prospective heart disease study such as the Holter Project underway at the University of Guelph. Enrolment in one of these studies will offer the owner an opportunity to determine if their dog is in the occult stage of DCM. If so, this will allow the owner an opportunity to start early therapy that will delay the progression of DCM. Thus, the most you can do to prevent your Dobe from getting DCM is to find out as soon as possible if your dog has occult DCM so you can start therapy ASAP to delay the progression of DCM.
What is Atrial Fibrillation?
Atrial fibrillation is a chaotic rhythm disturbance that is usually part of
DCM. We often observe that Dobermans in the occult stage of DCM progress to the overt stage of DCM (that is congestive heart failure) with the
development of atrial fibrillation. Thus atrial fibrillation is usually an
added complication of DCM that pushes dogs into heart failure. Atrial fibrillation is a more common complication of Dobermans with DCM than
with DCM in other breeds of dogs.
Why is atrial fibrillation an issue for Doberman Pinschers?
Dobermans with atrial fibrillation and DCM die sooner than Dobermans with DCM without atrial fibrillation. Recall that the average survival for Dobermans with DCM and congestive heart failure and no atrial fibrillation is 90 days.
If my dog has a Holter or cardiac ultrasound and it is normal does this mean he will not get DCM?
A normal exam today (be it by Holter or cardiac ultrasound or even routine ECG [however, this is markedly inferior to the other two tests]) does not ensure that the dog will be normal for the rest of his/her life. 25% of our dogs that developed DCM were over 10 years of age. Nevertheless this is the best you can do at this time. Our work indicates that it is profoundly unlikely that a dog that passes on one of these two exams with develop DCM within the next two years. Beyond two years we can not predict at this time. Thus all symptom fre
e Dobermans should be in a yearly screening program.
Breeder/Exhibitor Ed, Health
CHOCOLATE POISONING
Chocolate contains theobromine – a substance toxic to dogs. Baking chocolate contains more theobromine per ounce than semisweet chocolate, which, in turn, contains more theobromine than milk chocolate. While most lethal cases of chocolate poisoning occur when small dogs eat large quantities of baking chocolate, owners should nonetheless keep their dogs and chocolates well-separated.
If you witness your dog eating chocolate or if it shows any signs of chocolate toxicity (anxiety, pacing, hyper-excitability, excessive thirst and urination, vomiting, or seizures): call your vet immediately and tell him or her what type of chocolate your dog ate, how much you think it ate, how long ago it indulged itself, and how much your dog weighs.
If you find your dog within a couple of hours of ingesting the chocolate you can administer peroxide to the animal by mouth to induce vomiting. Hydrogen peroxide 3% is the emetic of choice for dogs and can be dosed at 15 ml in dogs up to 40 pounds and 30 ml in dogs less than 40 pounds. If you can reach your vet he will either instruct you on how to do administer the peroxide or ask you to bring your dog to the clinic to have its stomach pumped.
If more than a couple of hours have passed the toxin will already be circulating in your dog´s system so your vet will provide supportive therapy (such as intravenous fluids and drugs to control hyper-excitability) while your dog´s body works to detoxify itself.
FEBREZETM – IS IT TOXIC TO YOUR PET?
- ASPCA National Animal Poison Control Center
- 1717 S. Philo Road Suite 36 Urbana, IL 61802
Date: March 26, 1999
To: Whom It May Concern
there have been comments and discussions posted on the Internet suggesting that the use of FebrezeTM Fabric Refresher in households is dangerous to animals. We have issued the following statement in order to help disseminate accurate information:
“Veterinary toxicologists at the ASPCA National Animal Poison Control Center are conducting an on- going investigation into claims that use of FebrezeTM in the home caused the death of several pets. All information reviewed to date suggests that there is no evidence that FebrezeTM represents any risk to pets when used according to label instructions. Presently, the center considers the product safe to use in households with pets.
As with any cleaning product, the center recommends that birds be removed from the room until the product application has dried and the area has been ventilated.
Please call 1-800- 345-4735 if you have any questions or have a pet that you suspect is experiencing problems or visit us at http://www.napcc.aspca.org.”
ICE MELTS AND ROCK SALTS – PET HEALTH HAZARDS
Pets may be exposed to ice melts that have been spilled, applied to sidewalks, or improperly stored. The most common clinical signs are vomiting. Other effects include diarrhea, salivation, depression, and loss of appetite, disorientation, increased thirst, seizures and even death.
Before initiating treatment for ice melt products, it is critical to know the ingredients and the animal´s health status. Electrolyte levels should be taken to determine the possible toxin.
Inducing vomiting is controversial if the product contains large amounts of potassium chloride. Activated charcoal does not absorb the salts in ice melts.
If an animal walks on or rolls through the product, etc. bathe the pet and monitor it for skin irritation. Also monitor and correct abnormalities in hydration status, electrolyte concentrations, and heart muscle activity.
There are many brands of de-icing products on the market. The most common ingredients in these ice melts are sodium chloride, calcium carbonate, and calcium magnesium acetate. A few ice melts contain urea.
Sodium Chloride
Sodium toxicosis is possible after large ingestion of ice melts, salt, or rock salt. A dose of 4grams per kilogram (2.2 pounds) of sodium chloride can be lethal in dogs. Ingesting large amounts of sodium levels can be lethal in dogs. Ingesting large amounts of sodium can lead to increased urination. Large amounts of ingested sodium can also lead to swelling of the brain. Also, the digestive upset along with the increased urination may lead to dehydration, further worsening the patient´s condition.
The clinical signs of sodium toxicity are primarily neuroligic. The severity of the signs is related more to the suddenness of onset rather than the magnitude of signs.
Diagnosis of sodium toxicosis is based on serum concentrations and a history of sodium ingestion.
Treatment goals are to replace water and electrolytes. Diuretics may also be of some use. The fluid of choice is 5% dextrose IV. The diuretic recommended is furosamide.
Potassium Chloride
Signs associated with elevated potassium levels include muscle weakness, GI disturbances, and cardiac conduction disturbances. Ingestion of potassium chloride tablets has caused bowel strictures and ulceration.
Treatment includes administration of lactated ringers and furosamide. Due to the irritating nature of potassium chloride-induction of vomiting is controversial. Activated charcoal does not bind potassium.
Magnesium Chloride
Elevated magnesium concentrations can cause low blood pressure and cardiac abnormalities, weakness, and neurological signs.
Treatment is symptomatic and supportive. Vomiting may reduce the amount of absorption if induced with in two hours of ingestion.
Calcium Carbonate and Calcium Magnesium Acetate
These products may cause vomiting and eye irritation. Treat gastric upset symptomatically.
Urea
This product is more toxic to ruminants (cows) than monogastric animals (dogs, cats, people). Ingestion of urea by dogs usually results in local irritant signs such as hyper salivation, GI signs of vomiting, and abdominal pain.
Treatment includes inducing vomiting and monitoring the animal.
According to National Animal Poison Control (800 548 2423) an alternative to the salts is sand or kitty litter. Also, of the ice melts available-those containing sodium chloride are the least toxic.
Again-most of the danger comes from ingestion of the products
LAWN CARE PRODUCTS
LAWN CARE PRODUCTS Lawn care products have been a concern to pet owners for many years. The public is under the impression that these products are primarily pesticides, and that they are very toxic or pose a significant health threat. Here are some common questions and the answers about lawn care products.
HOW CAN YOUR PET BECOME EXPOSED TO LAWN CARE PRODUCTS? The two most common routes of exposure are orally and dermal. Exposure to liquid concentrates and granules are possible with homeowner storage. Exposure to the diluted liquids is possible during application or before foliage drying. Exposure to applied granular material usually is the result of spills during loading equipment´s, spreader equipment failure, or spreading granules on non-lawn surfaces such as driveways and sidewalks.
DOES EXPOSURE RESULT IN TOXICOSIS? Intoxication from these products is dose related. In most cases, exposure will not result in any adverse effects, there are some exposures that could. Consumption of liquid concentrates while mixing or granules in storage in more likely to result in toxicosis than any
other common exposure. This is because of the higher chemical concentration and total amount of product available to the animal. Consumption to excessive amounts of granules such as in driveways or from spills may result in mild clinical signs. Oral or skin exposure to lawns where diluted liquids or granules are properly applied generally are of negligible risk. This statement is made when considering (1) the low chemical concentration of the liquid application, (2) the large area of application, (3) low liquid volume applied per unit area of lawn, (4) low percentage of dislodgeable chemical residue from foliage, (5) granular deposition in the thatch layer, and (6) less the exposed dose. The exposed dose is then often compared to the no observable effect level (NOEL) determined in the chronic experimental studies and other experimental forensic data.
DO LAWN CARE CHEMICALS CAUSE CANCER IN ANIMALS? Long-term chronic experimental studies in dogs do not support the conclusion that the chemicals identified in table 1 are carcinogenic. The only scientific data that are in conflict with that conclusion is the much publicized work of Hayes et al. (1992). It is the author´s opinion that serious flaws in this epidemiological study have negated the conclusions of this study. Unfortunately, there are no other epidemiological studies.
WHAT INFORMATION DO I NEED TO STRONGLY SUSPECT LAWN CARE CHEMICAL TOXICITY? The clinical signs and clinical history must be compatible with specific chemical exposure . In the case of death, a post-mortem examination should reveal the appropriate chemically related target tissues, and gross and histopathologic findings. The amount of chemical in the exposure must be sufficient to cause adverse effects. Any clinical pathologic findings should be compatible also. An example would be an alleged acute organophosphate-related death depression of brain cholinesterase. Exposure alone is not sufficient evidence to diagnose intoxication. Currently, in most cases, there is not enough information available for these chemicals to determine an expected lethal or toxic concentration in tissues or body fluids. Therefore, the analytical findings of a chemical in animal tissue or body fluids is evidence of exposure but not necessarily intoxication
IS THERE A TOXICOLOGICAL CONCERN ABOUT INERT INGREDIENTS? Since the majority of the applied liquid products are soluble in water and are diluted when mixed with water and are diluted when mixed with water, inert ingredients in the products themselves are of little concern. In general, the inert ingredient in granular products also not of toxicological concern.
IS THERE A CONCERN ABOUT MIXTURES? There are not many good experimental studies using standard mixtures of these products. Because most of these products have different mechanisms of producing toxicity and based on current experimental work with mixtures, it does not appear that most mixtures result in toxicological potentiation or synergy.
WHY DOES POSTING OF LAWN APPLICATIONS OCCUR? In many states and localities, positing of lawn care product application is required by law. Posting serves s a notification that lawn care application occurred. It is part of the community´s right to know. Posting is not related the toxic potential of materials used.
WHY IS IT RECOMMENDED THAT ANIMALS AND HUMAN STAY OFF LAWNS UNTIL LIQUID APPLICATIONS DRY? It is recommended that animals and humans stay off the lawn until the liquid application is dry to limit exposure. As with any chemical (e.g., lawn care product, detergent), there should be an effort by the public to limit exposure. The amount of chemical that is dislodgeable decreases as the liquid dries. The overall difference between the actual exposure dose and a toxic dose is changes little by foliage drying; therefore, the risk is still negligible without drying.
Breeder/Exhibitor Ed, Health
Shock is lack of adequate blood flow to meet the body’s needs. Adequate blood flow requires effective heart pumping, open intact vessels and sufficient blood volume to maintain flow and pressure. Any condition adversely affecting the heart, vessels or blood volume can induce shock.
At first the body attempts to compensate for the inadequate circulation by speeding up the heart, constricting the skin vessels and maintaining fluid in the circulation by reducing output of urine. This becomes increasingly difficult to do when the vital organs aren’t getting enough oxygen to carry on these activities. After a time, shock becomes self-perpetuating. Prolonged shock causes death.
Common causes of shock are dehydration (prolonged vomiting and diarrhea), heat stroke, severe infections, poisoning and hemorrhage. Being hit by a car is the most common cause of traumatic shock in the dog.
Transporting a dog in shock. Muzzle only when absolutely necessary. (J. Clawson)
The signs of shock, which are caused by the effects of poor circulation and the adjustments made to compensate for this, are a drop in body temperature; shivering; listlessness and mental depression; weakness; cold feet and legs; pale skin and mucus membranes; a weak faint pulse.
Treatment: First evaluate the signs present. Is the dog breathing? Is there a heartbeat? What are the extent of the injuries? Is the dog in shock? If so, proceed as follows:
1. If not breathing, proceed with artificial respiration.
2. If no heartbeat or pulse, administer heart massage.
3. If unconscious, check to be sure the airway is open; clear secretions from the mouth with your fingers; pull out the tongue to keep the airway clear of secretions. Keep the dog’s head lower than the body.
4. Control bleeding (as described under Wounds section that follows).
5. To prevent further aggravation of shock:
a. Calm your dog and speak soothingly.
b. Let the dog assume the most comfortable position, and adopt the one with the least pain. Don’t force your dog to lie down-it may make breathing more difficult.
c. When possible, splint or support broken bones before moving the dog (see MUSCULOSKELETAL SYSTEM).
d. Cover your dog with a coat or blanket. Do not wrap tightly.
e. Transport large dogs on a flat surface or in a hammock stretcher. Carry small dogs with injured parts protected.
f. Muzzle only when absolutely necessary. It may impair breathing.
WOUNDS
In the care of wounds, the two most important objectives are first to stop the bleeding, and then to prevent infection. Since wounds are painful to the dog, be prepared to restrain or muzzle before you treat the wound.
Control of Bleeding
Bleeding may he arterial (the spurting of bright red blood), or venous (oozing of dark red blood), or sometimes both. Do not wipe a wound that has stopped bleeding. This will dislodge the clot. Don’t pour hydrogen peroxide on a fresh wound. Bleeding then will he difficult to control.
The two methods used to control bleeding are the pressure dressing and the tourniquet:
The Pressure Dressing: Take several pieces of clean or sterile gauze, place them over the wound and bandage snugly. Watch for swelling of the limb below the pressure pack. This indicates impaired circulation. The bandage must be loosened or removed.
Apply pressure over the artery in the groin to control arterial bleeding in the leg. (J. Clawson)
An alternate method to control bleeding is to apply pressure over the artery in the groin or axilla. (See CIRCULATORY SYSTEM: Pulse). Often this will control bleeding long enough to permit an assistant to apply a pressure dressing.
If material is not available for bandaging, place a pad on the wound and press it firmly. Hold in place until help arrives.
The Tourniquet: A tourniquet may be needed to control a spurting artery. It can be applied to the tail or leg above the wound (between the wound and the heart). Take a piece of cloth or gauze roll and loop it around the limb. Then tighten it by hand, or with a stick inserted beneath the loop and twisted around until bleeding is controlled. If you see the end of the artery, you might attempt to pick it up with tweezers and tie it off with a piece of cotton thread. When possible, this should be left to a trained practitioner.
A tourniquet should be loosened every thirty minutes for two to three minutes to let blood flow into the limb.
Treating the Wound
All wounds are contaminated with dirt and bacteria. Proper care and handling will prevent some infections. Before handling a wound, make sure your hands and instruments are clean. Starting at the edges of a fresh wound, clip the hair back to enlarge the area. Cleanse the edges of the wound with a damp gauze or pad. Irrigate the wound with clean tap water. Apply antibiotic ointment. Bandage as described below.
Older wounds with a covering of pus and scab are cleansed with 3% hydrogen peroxide solution or a surgical soap. Blot dry. Apply antibiotic ointment and bandage as described below.
Dressings over infected wounds should be changed frequently to aid in the drainage of pus, and to allow you to apply fresh ointment.
Fresh lacerations over one-half inch long should be sutured to prevent infection, minimize scarring and speed healing. Wounds over twelve hours old are quite likely to be infected. Suturing is questionable.
Bites are heavily contaminated wounds. Often they are puncture wounds. They are quite likely to get infected. They should not be sutured. Antibiotics are indicated.
With all animal bites, the possibility of rabies should be kept in mind (see Infectious Diseases: Rabies).
Bandaging
The equipment you will need is listed in the Home Emergency and Medical Kit, in the photo at the beginning of this chapter.
Foot and Leg Bandages. To bandage the foot, place several sterile gauze pads over the wound. Insert cotton balls between the toes and hold in place with adhesive tape looped around the bottom of the foot and back across the top until the foot is snugly wrapped.
A method of applying a foot bandage for a lacerated pad. Tape loosely to allow good circulation. (J. Clawson)
A sock slipped over a gauze square is a good bandage for ease of dressing change.
For leg wounds, begin by wrapping the foot as described. Then cover the wound with several sterile gauze pads and hold in place with strips of adhesive tape. Wrap the tape around the leg but don’t overlap it so that the tape sticks to the hair. This keeps the dressing from sliding up and down, as often happens when a roll gauze bandage is used. Flex the knee and foot several times to be sure the bandage is not too tight and there is good circulation and movement at the joints.
When a dressing is to be left in place for some time, cheek on it every few hours to be sure the foot is not swelling. If there is any question about the sensation or circulation to the foot, loosen the dressing.
Many-Tailed Bandage. This bandage is used to protect the skin of the neck or abdomen from scratching and biting and to hold dressings in place. It is made by taking a rectangular piece of linen and cutting the sides to make tails. Tie the tails together over the back to hold it in place.
A many-tailed bandage may be used to keep puppies from nursing
infected breasts.
Eye Bandage. At times your veterinarian may prescribe an eye bandage in the treatment of an eye ailment. Place a sterile gauze square over the affected eye and hold it in place by taping around the head with one inch adhesive. Be careful not to get the tape too tight. Apply the dressing so that the ears are free.
You may be required to change the dressing from time to time to apply medication to the eye.
The ear bandage is discussed in the chapter EARS.
Elizabethan Collar – An Elizabethan Collar, named for the high neck ruff popular in the reign of Queen Elizabeth. It is a useful device to keep a dog from scratching at the ears and biting at a wound or skin problem. They are recommended for certain disorders discussed in the SKIN chapter. They can be purchased from some veterinarians or pet stores, or can be made from plastic and cardboard. Plastic Flowerpots, wastebaskets and buckets work well.
Elizabethan Collar. (J. Clawson)
The size of the collar if tailored to the dog Cut just enough out of the bottom to let the dog’s head slip through, then fasten the device to a leather collar by strings passed through holes punched in the sides of the plastic. The neck of the collar should be short enough to let the dog eat and drink. Most dogs adjust to them quite well after a few minutes. Others won’t eat or drink with the collar in place. In that case, temporarily remove the collar.
Breeder/Exhibitor Ed, Health
by Marj Brooks, Manorie Dobermans, USA
In its basic form, this was posted to DQ by Marj Brooks. We’ve tried it on a blue bitch puppy that had horrid skin and coat problems. The results were almost immediate and all were positive. We make no claims to its effectiveness other than the fact that it worked for us.
B-Complex
We use B-50’s. The vitamins are mostly in equal amounts…..especially the B-2 and B-6. We gave one tab, FOUR TIMES A DAY as prescribed in the DQ. We tried cutting down to two a day on these, because of her age, and immediately saw a turn for the worse. After upping it to THREE, the success curve went dramatically upwards. We found that, for a puppy of eight months, THREE a day was sufficient. I would highly recommend using FOUR on an adult…..or at least a dog of 12 months +.
Brewers Yeast
Marj’s article recommend 7-grain. We had difficulty locating 7-grain, but easily found 10-grain. As opposed to the original directions of giving one 7-grain four times a day, we went with one 10-grain THREE times a day. It appears to have been successful.
Folic Acid
The recipe in DQ called for 1-mg, prescription size tabs, 1/4 tab, four times a day. It’s proved to be very effective to use the 1/4-meg size (250mcg) and administer accordingly = ONE TAB FOUR TIMES a day.
Additions
In addition to the above formula, we also include ONE Ester-C tab daily, in place of straight Vit. C; and ONE Chelated Zinc tab (50-mg) for total flea control.
Conclusions
The blue bitch puppy involved with this recipe not only had a “typical blue coat” , but was affected with generalized Demodex; thereby having extremely DRY skin from the get-go. She was dipped in Mitaban medication on a weekly basis, which added to the inordinately dry condition of the skin and coat.
Within 10 days of putting her on this ‘recipe’, the surprising results were obvious to even the casual observer. Her coat took on a silky-like appearance, her skin no longer resembled elephant hide, the actual hairs in her coat felt thicker and softer to the touch……and the coat darkened considerably.
When we attempted to reduce the amount of the B-Complex (by 1/2) because of her age, it only took three days for us to see that she was beginning to dry out at pressure points. After increasing the dosage by ONE tab daily, the dryness began to disappear. We’ve kept her at that dosage level and have seen no digression to the previous dry condition. Please note that the B-Complex also has small dosages of Folic Acid. I believe the Folic Acid plays a VERY big part in the success of this formula.
Disclaimer
We highly recommend this recipe, but as stated above, claim no responsibility for either its success or failure. All dogs are not the same and therefore, do not react the same to medications and/or supplements. We are not vets and do not assume to be giving directions to ANYONE regarding their dog’s health or physical conditions.
Breeder/Exhibitor Ed, Health
written by Robert Hart, Vitality Science
Who doesn´t love fried foods? Fried chicken, fried fish, chicken fried steak, fried veggies; lunches and dinners are often accompanied with fried; potato chips, corn chips, tortilla chips, french fries, onion rings… Detail breaks often include meeting fellow officers for donuts and coffee. The tastier donuts are deep-fried- Of course!
The FDA estimates the average American eats 4.7 pounds of trans-fats each year!
The two primary reasons why doctors caution against eating fried foods are:
- Since saturated fats are impossible to process, they clog the liver and arteries (early on causing GI issues, and over time immune disorders/diseases).
- High heat destroys any nutritional value the food might have started with; High heat also chemically changes trans-fat oils into potential carcinogens.
Fast Food restaurants are in business to make a profit. Instead of replacing spent oil with fresh oil, they simply top off the fryers with fresh oil.
If you like fried foods that much, eat them at home, where you control the quality of the oil (coconut is very good), as well the cooking time and temperature. CAUTION: Do not reuse the spent oil!
Eventually though, all restaurant fry oil (and fry grease) gets dumped and replaced. Ever wonder what becomes of it?
The law requires all restaurants to have grease traps. The more fried food cooked, the faster the grease traps fill up. Grease removal service is big business. But what do the Grease Haulers do with it?
They “Recycle it”! Grease Haulers make even more money “recycling” the grease from these traps. What could this rancid, carcinogenic, artery and liver clogging goop possibly be used for- an alternative bio-fuel perhaps? No, not exactly.
Here´s a trick question: What could possibly be worse than ingesting 4.7 pounds of high temperature trans-fat oils per year?
So what is the connection to your K-9 partner?
A dirty little secret of the dry pet food industry is that they buy the spent oil! Why? Hint- it´s not to power their generators!
The competition for the pet food dollar is fierce. Each company is outdoing the next with ever more eye-catching packaging. If you have a working knowledge of nutrition, you will be appalled at what is inside the bags.
Dry pet food is extruded under high heat and pressure, destroying any nutritional value it might have started with. And, if that´s not bad enough, the so-called vitamins and minerals they include are the poorest quality, least beneficial, yet they meet the legal requirements to be included as ingredients.
Alas, if their multi-billion dollar advertising budgets were spent on the contents, dogs would be a lot healthier. Buyers beware!
Did you ever wonder what the oily residue was that gets all over your hand if you don´t use a scoop to get the dry food from bag to bowl? Recycled grease and fry oil are actually sprayed on -to give this otherwise tasteless, nutritionless bulk some “flavor”!
If you´re wondering why the FDA hasn´t stepped in, the fact is most of the human dry foods on grocery store shelves are as bad. It seems that the FDA is a feel good government agency that lobbyists steam-roll over.
Don´t think for a minute that canned foods are much better; they´re not! The sickest feed lot animals, those that do not sneak by the meat and poultry inspectors, are sold to dog food manufacturers.
Food digestion is a time sensitive process; too long, or too short leads to health issues. Meals that lack nutritional value are difficult to process. There´s a big difference in an occasional fast-food meal versus a steady diet of fast foods. Over time, a steady fast-food diet leads to health problems.
The movie “Super Size Me” is well worth renting. Your health, and that of your K9 partners´, may depend on you watching it.
“Fully 90% of all disease is caused by an unhealthy intestinal system” Royal Society of Medicine Great Britain
It is no coincidence that today, tens-of-millions dogs are dealing with the same diseases that we are! During the last 40 years, a frequent diet for police officers (and their K-9 partners) has become fast food.
Early warning signs include skin disorders, gas, bloat, abnormal bowel movements. Over time, more advanced GI and immune disorders/diseases develop.
At least 5 generations of domestic dogs have been raised from weaning to the grave on dry foods. Each generation is genetically weaker. Today, many breeds are born with severely compromised GI and immune systems. Failure to thrive, hip displasya, and cancer are but a few examples of compromised immune systems in German Shepherds.
The good news: Most diseases can be reversed (or prevented), especially in dogs. Why dogs more than us? Well, unless you give them junk food treats (dog or human), once you improve their diet, they can´t cheat. Recovery signs follow quickly as vital GI and immune defense systems are reestablished.
You Can Domesticate The Dog, But Not It´s Diet!
To know what the best diet is for your dogs, you only have to observe their wild relatives.
Feral animals instinctively supplement their fresh kill diet by eating grass and dirt for the microflora and soil based microorganisms (SBOs) that are essential digestive aids.
Pesticides, insecticides, chemical run off, and chlorinated lawn water have effectively killed SBOs. Today, these essential digestive aids are grown in environmentally controlled laboratories.
Drinking water is often overlooked as a health risk. Obviously, you don´t want your dog to drink from a puddle, but municipal water contains large quantities of Chlorine, to kill a growing list of pathogens. If your dog drinks enough of it, it will kill the good bacteria he needs!
By the way, antibiotics are indiscriminate killers; they kill off the essential food processing bacteria, as well as the ones causing GI issues. Most of time, all your K-9 needs is a few extra doses of SBOs to overcome a GI problem. An added bonus is that SBO administration does not require withholding food or water!
If you want to make sure your K-9 partner stays healthy, introduce a more natural diet.
No matter what you feed your dogs, if you supplement each meal with essential digestive enzymes, vital oils, and SBOs you will soon have a healthier, happier, more mentally alert and physically stronger K-9 partner.
If your K-9 partner is not responding to improved diet and supplement, chances are the intestinal wall is inflamed. The intestinal wall is your K-9s lifeline. This is where nutrients are absorbed into the body, AND, where waste products are dumped into the intestines for elimination.
If the intestinal wall becomes inflamed, this vital nutrient/waste exchange cannot take place. When that happens, your K-9 partner is not only not getting the nutrition it is desperate for, waste products are building up and recycling throughout its´ body, making him sicker. Natural anti-inflammatories need to be administered before the benefits of any medication, or diet changes will have a positive effect.
Nutritious food, clean water, and essential supplements are vital to maintaining and restoring optimum K-9 performance.
The author of this article is Robert Hart, co-founder of Vitality Science, Inc. The company formulates natural alternatives to restore and maintain optimum K-9 health and performance. Vitality Science had a booth at K-9 Magazines February 07 Seminar in Orlando.
Breeder/Exhibitor Ed, Health
How your dog benefits from rawhide and how to choose the correct chew for your dog…
For centuries, wild canines and their predecessors chewed on the hides of their hoofed prey. Chewing the tough hide provided cleaning action for teeth, exercise for gums, and a source of sport for the young. Only since 1959 have we recognized the dog’s natural desire to chew animal skin and its benefit to domestic dogs.
What is rawhide?
Rawhide is the inner layer of the hide of any cleft-hoofed bovine livestock. Beef hide is premium rawhide made from cows raised for consumption. American beef hide is derived from corn-fed cows within U.S. borders.
What makes rawhide so tough?
Collagen fibers link to make the hide tough yet flexible. Human skin has the same basic structure, but is much thinner.
Where does it come from?
The quality of rawhide is often related to its country of origin:
Oriental Water Buffalo – Raised to work in the fields of countries like China, Thailand, and Korea, they are a common source of rawhide.
South American Range Cows – These animals are fed on grass and typically have little fat and a rough, fibrous consistency. They are warm-weather animals with a thinner skin.
American Beef hide – Corn-fed beef raised in the U.S. supply a thick, palatable, and high-quality chew. American beef hide is considered “the source” of choice for premium chews.
What is it made from?
The animal’s skin is split into inner and outer layers. The tough outer layer is used for leather shoes, garments, and upholstery, while the softer inner layer is cut and formed into different shapes for dog chews.
How is it processed?
The animal’s hide is transported to processing plants where it is split, washed, and cleaned. The hides are then cut, formed, and dried into the many varieties of rawhide you see in the stores.
In less developed countries, a lack of modern roads and refrigerated trucks often requires the use of preservatives to get skins from some outlying areas to processing plants. In the U.S., fresh beef hides are refrigerated during shipping to prevent degradation and avoid preservatives.
Will my dog chew such a hard rawhide?
When collagen in the skin dries out, it becomes stiff. As your dog chews, the saliva moistens and softens the rawhide. Foreign rawhide is often sun parched, while U.S. beef hide is oven dried to prevent over-drying. Smooth, shiny areas on a chew are a sign of heat breakdown and should be avoided.
How can chews help my dog?
Chews offer two valuable benefits to your dog:
Dental Benefits
Infections, kidney, and heart disease can result when poor dental health gives bacteria a channel to enter your dog’s body.
Bacteria in the dog’s mouth break down food particles and convert them to plaque and excess acid. This plaque can become mineralized to form a hard deposit on the tooth surface called “calculus”. The excess acid damages the gums, resulting in gingivitis. Unchecked gingivitis results in periodontitis, the leading cause of tooth loss.
As rawhide is chewed and moistened, it wraps around the teeth and rubs off plaque and calculi. Wild hunting canines tore through their prey’s skin with their canines (front teeth). Modern dogs chew most foods and beef hide with their molars (back teeth), leaving the canine teeth susceptible to plaque and calculus buildup.
Rawhide’s cleaning effect
New research from Harvard University has conclusively proven the dental benefits of chewing rawhide.
Cleaner teeth mean fresher breath
Most bad breath in dogs is caused by gum disease. Inflamed gums, plaque, and calculus harbor the bacteria that creates mouth odor. Even young dogs need dental care – 85% of dogs two years old or more have some periodontal disease. Ask your veterinarian about a program to keep your dog’s teeth clean.
Veterinarian’s role in dental health
Tooth care is crucial to your dog’s health. Your dog’s teeth should be examined by a veterinarian yearly, and cleaned and polished as needed. Veterinarians recommend daily brushing to prevent plaque buildup. Use beef hide chews daily to supplement brushing. Harper’s Dental Chews are specially formulated to reduce the formation of plaque.
Choosing the Correct Chew
Types of Chews:
Best for:
1. BASTED RAWHIDE/BEEF HIDE
Chicken, beef, or other coatings make chews tastier to your dog. Most of these coatings are water-soluble and do not stain. Very, very choosy dogs
2. GROUND RAWHIDE CHEWS
These chews come in all shapes and colors and consist of ground rawhide held together with a binder.
Choosy dogs, dogs with sensitive mouths
3. AMERICAN BEEF HIDE CHEWS
Made from U.S. feeder cattle. It is the premium chew because of its consistency, softness, and taste.
Most healthy dogs
4. RAWHIDE CHEWS
Made from water buffalo, range cows, and others.
Aggressive chewers
5. PRESSED RAWHIDE CHEWS
Made from layers of skin pressed together by machine. It is very hard.
Very aggressive chewers
Choosing size and shape
Your dog’s preference will vary with different beef hide shapes. Fortunately, chews come in every size and shape imaginable. It is important that the chew be large enough and thick enough that your dog cannot easily chew off and swallow a large piece or the whole chew. Rawhide that requires more than 7 days to chew should be replaced due to dirt and bacteria buildup.
Which dog should not have chews?
If your dog has gastrointestinal disease or is eating a therapeutic diet, you should seek a veterinarian’s approval before feeding chews. Dogs with beef allergies or that consistently swallow bones whole should probably not receive chews.
How often should I feed chews?
Rawhide is not a food, but a safe, chewable toy. It is high in protein, low in fat, and has fewer calories per ounce than a typical dog biscuit. An hour of chewing daily is a good rule for thumb for feeding chews.
Shop for Quality
* Select
Thick rawhide/beef hide that lasts.
* Avoid
Paper-thin, tightly wrapped chews with sharp edges.
* Select
Beef hide with natural color variations.
* Avoid
Over-processed chews with a stark white or whitewashed surface.
Breeder/Exhibitor Ed, Health
 |
Dr. Peggy Root Kustritz is a 1987 graduate of the University of Minnesota College of Veterinary Medicine. She currently is employed as a clinical specialist in small animal reproduction at the University of Minnesota College of Veterinary Medicine .
|
Dogs and human males are the only beings that suffer from prostate disease commonly. This is to our advantage, as dog enthusiasts, because much research has been done on prostate disease in dogs in an attempt to better understand it in humans.
The prostate is a gland that encircles the neck of the urinary bladder . Multiple small ducts penetrate the urethra at the site of the prostate, allowing prostatic fluid to intermix with spermatozoa as they are ejaculated, to create semen. Dogs have no other accessory sex glands and, therefore, no other source of seminal fluid; all fluid present in the ejaculate arises from the prostate. Prostatic fluid is secreted at all times, whether the dog is being used for breeding or not. Most accumulates in the urinary bladder and is voided with the urine. Some runs down the urethra and accumulates at the opening of the prepuce, forming the mass of greenish discharge that often is visible on intact male dogs.
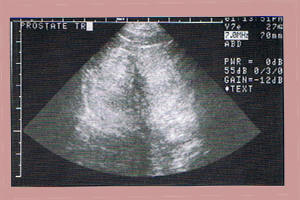
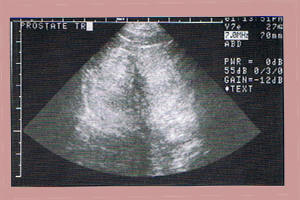
Diagnostic tests used to determine if prostate disease is present and, if so, type and extent of that disease, are the same for all conditions. Rectal palpation of the prostate can be used to assess prostatic size, shape and consistency and to determine if the dog is painful when the prostate is manipulated. Because the prostate encircles the neck of the urinary bladder, which is freely movable between the pelvis and abdominal cavity, an enlarged prostate may pull the bladder too far into the abdomen to be palpable per rectum. Some extremely enlarged prostates can be felt on abdominal palpation, Radiography has been used historically as a diagnostic test for prostate disease but ultrasonography is the technique employed most often at this time. Ultrasonography allows the operator to look through the prostate and guides placement of the needle or biopsy instrument if samples are to be collected directly from the prostate (Figure 2). Because all the fluid in the ejaculate arises from the prostate, semen can be collected and samples submitted for culture and microscopic assessment. Specific results of these diagnostic tests will be described with each disease.
Measurement of proteins in serum, as is used in human medicine, has not been shown to be consistently effective either for diagnosis of canine prostate disease or for determination of adequacy of treatment. Prostate specific antigen (PSA), commonly tested in human males, is secreted in dogs but concentrations do not vary predictably with presence or absence of prostate disease. Blood testing is not a common component of prostate evaluation in dogs at this time.
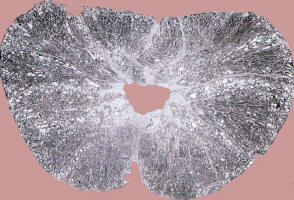
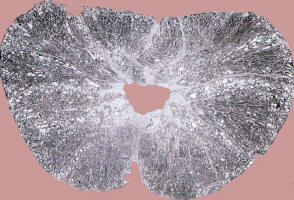
The predominant male reproductive hormone, testosterone, is metabolized in the body to form dihydrotestosterone (DHT). This secondary compound gradually causes an increase in size of the prostate gland such that all intact male dogs (and all human males) eventually have some degree of prostate enlargement. Prostate disease is fairly common in dogs, with a reported incidence of 2.5%. The average age at which prostate disease becomes clinically evident is 9 years. (Figure I – Prostate tissue, microscopic view. The central V-shaped area is the urethra) The prostate diseases most common in dogs are benign prostatic hypertrophy/hyperplasia (BPH), prostatitis and prostatic abscesses, prostatic cysts and prostatic neoplasia.
|
|
- Figure 1 – Prostate tissue, microscopic view.
- The central V-shaped are is the urethra.
|
Benign Prostatic Hypertrophy/ Hyperplasia (Bph)
Benign prostatic enlargement consists of both hypertrophy (increase in size of prostatic cells) and hyperplasia (increase in number of prostatic cells). This occurs gradually with age and continuing exposure to the hormone DHT. In one study, 50% of dogs examined had some evidence of BPH by 4 to 5 years of age. Because this condition is dependent on continuing hormone secretion, it is seen only in intact dogs.
Many dogs with BPH show no clinical signs of disease. The most common clinical sign in dogs is dripping of bloody fluid from the penis unassociated with urination. Since prostatic fluid accumulates in the urinary bladder, bloody urine also may be seen. Occasionally, blood in the semen is the first problem noted by owners. In all other respects, dogs with BPH are normal. This differs from men, who are most likely to describe frequent passage of small amounts of urine as their primary complaint. Other signs that may be seen in dogs are referable to the greatly increased size of the prostate and include rectal tenesmus 9excessive straining to defecate) and subsequent passage of ribbon-shaped feces.
On rectal palpation, the prostate of dogs with BPH is symmetrically enlarged and non-painful. When examined by ultrasound, the prostate is enlarged but the tissue is uniform in appearance (Figure 3). The prostatic fluid, usually collected by manual ejaculation of the dog, is not inflammatory and semen cultures arc not significant.
No treatment is necessary for dogs with no clinical signs of BPH. The presence of BPH predisposes dogs to prostatitis so it should not be ignored; diagnostics for prostatitis should be performed periodically by your veterinarian (see below). Semen containing blood may be sufficient to effect pregnancy when bitches are bred by natural service or artificially inseminated with fresh semen but bloody semen should not be used for chilled or frozen semen, even if the sample is centrifuged and the bloody prostatic fluid removed immediately. Survival of spermatozoa ejaculated into bloody prostatic fluid is poor when those spermatozoa are stored for any length of time.
The best treatment is castration. Removal of the testes causes an abrupt decline in testosterone concentrations with subsequent lack of DHT. No medical therapy is as ef
fective as castration as a treatment for BPH.
For valuable breeding dogs, medical therapy may be necessary, at least until enough semen can be frozen to ensure the dog’s genetics are still available for future breedings. Herbal therapies used in humans, for example saw palmetto extract, have been shown not to be effective in dogs. Estrogen therapy has been described historically for treatment of BPH. The author does not recommend this therapy. While it may decrease clinical signs of BPH, it decreases the secretory function of the prostate, predisposing it to infection and may be detrimental to production of spermatozoa.
|

|
|
Figure 2 – Performance of ultrasound guided collection of cells from the prostate
|
Progesterone therapy also has been described, with either injectable or oral forms of progesterone reported to effectively decrease prostate size and clinical signs of BPH without altering semen quality. Long-term progesterone therapy has not been described.
The drug therapy most recently described is use of finasteride, a human drug for BPH that acts by inhibiting formation of DHT from testosterone. ProscarTM is a 5 mg tablet of finasteride, approved for treatment of BPH in men. PropeciaTM is a 1 mg tablet of finasteride, approved for treatment of male pattern baldness in men, which also is due to DHT. Either medication can be used in dogs. Work done at the University of Minnesota and Washington State University by Dr. Kaitkanoke Sirinarumitr, Dr. Shirley Johnston and the author demonstrated that dogs with spontaneous BPH respond well to fairly low doses of this drug when treated for 1 to 4 months. The dose used was 0.1 to 0.5 mg/kg daily, which is one 5 mg tablet daily for dogs up to 50 kg in weight. There was no adverse effect on libido or semen quality. Humans are encouraged not to try to father children while on this drug. Studies have demonstrated no birth defects in pups sired by dogs on finasteride. It must be understood that BPH gradually will redevelop once finasteride therapy is withdrawn. Finasteride is the author’s medical treatment of choice for canine BPH.
Prostatitis / Prostatic Abscesses
Prostatitis is infection of the prostate. The reproductive and urinary tracts of dogs contain a certain number of bacteria at all times and the prostate is well designed to prevent movement of those bacteria into the gland. Any time infection of the prostate is identified, some underlying abnormality of the gland must be investigated. The most common condition underlying prostatitis is BPH. Because prostatitis occurs secondary to other conditions, it may be seen in intact or neutered dogs.
Acute prostatitis is recent infection. Dogs with acute prostatitis| often show pain when ejaculating and may cry out when urinating or defecating. They may have a fever with decreased appetite and poor attitude. On rectal palpation, the prostate is enlarged and may be asymmetrical and the dog shows signs of pain when it is compressed.
Chronic prostatitis is long-standing infection. These dogs feel well and often, poor semen quality is the only clue that infection may be present. Some dogs with chronic prostatitis present with recurring urinary tract infections as their only clinical sign. On rectal palpation, the prostate is enlarged, may be asymmetrical and is non-painful. This is the most common presentation of prostatic infection in dogs.
Prostatic abscesses are localized, walled-off areas of infection. They may cause significant asymmetry of the prostate on palpation. Dogs may appear healthy or may collapse with system-wide infection and shock if the abscess ruptures into the abdomen. Prostatic abscesses are uncommon.
Ultrasound may be useful in diagnosing prostatitis, especially if an abscess is present
|
|
|
Figure 3 – Ultrasound of a prostate with BPH
|
|

|
|
Figure 4 – Ultrasound of a prostatic abscess. Note the circular dark area offset by white crosses.
|
Most ultrasonongraphic changes seen in dogs with prostatitis are non-specific. Culture of seminal fluid or tissue aspirated directly from the prostate is the preferred diagnostic technique. Three types of cultures should be performed. Aerobic bacterial culture identifies those bacteria that live in air; these are the common names you know, such as E. coli and Strep. Because some bacteria are normal in the urethra, through which the semen flows during collection, some bacteria always will be cultured from a semen sample. A significant result is moderate to heavy growth of any single organism. Anaerobic bacterial culture identifies bacteria that cannot live in air; these are less common but cause more damage if they’re present. Mycoplasma culture identifies mycoplasmas and ureasplasmas, organisms related to bacteria. These are difficult to grow so the laboratory usually is unwilling to give your veterinarian an idea of quantity grown because they cannot differentiate low levels of growth due to technique problems from low levels in the sample from the dog. Because of this, it is difficult for your veterinarian to know the significance of mycoplasma results in all cases. If the author feels that a dog has prostatitis, based on all other parameters, and mycoplasma is the only organism grown, she will treat for it.
Antibiotic therapy is the primary treatment for prostatitis. The appropriate antibiotic must be chosen based on culture and sensitivity results; knowledge of the acuteness of the episode of prostatitis and information about movement of various antibiotics into the prostate gland. The prostate is surrounded with a tight capsule that effectively keeps antibiotics out of the prostate. In dogs with acute prostatitis, this capsule is functionally broken and any antibiotic will likely penetrate prostatic tissue well. In dogs with chronic prostatitis, an antibiotic must be chosen that can move through the prostatic capsule well. As a general rule, fluoroquinolone antibiotics (BaytrilTM, CiproTM) and trimcthroprim-sulfa antibiotics (PrimorTM) are effective against prostatitis. Owners should be aware that long-term use of trimethoprim-sulfa antibiotics may be associated with dry eye and/or anemia; concurrent administration of folic acid may decre
ase this effect,
Antibiotics must be administered for at least 3 to 4 weeks. Semen should be cultured one week and again one month after therapy to determine if infection is resolved. Therapy to combat the underlying cause of prostatitis, such as BPH, should occur at the same time. Once a dog has suffered from prostatitis, it is a good idea to recheck that dog with semen evaluation and semen culture every 6 months until he is castrated. Castration, and subsequent decrease in size of the prostate, greatly promotes resolution of infection. Prostatic abscesses usually are resolved surgically.
Prostatic Cysts
Two types of prostatic cysts have been described. True cysts, also called retention cysts, are accumulations of non-infected prostatic fluid in cystic spaces within the gland. Paraprostatic cysts are large, thin-walled, fluid-filled structures next to the prostate. With either condition, dogs may present with urinary tract signs (difficult urination, blood in the urine) or gastrointestinal signs (lack of appetite, abdominal distension). These are easily diagnosed by ultrasound and are resolved surgically. Prostatic cysts are uncommon.
Proslatic Neoplasia
Prostatic neoplasia, or cancer, always is malignant and aggressive. Usually by the time the owner has noted clinical signs, the cancer has spread from the prostate into the lungs or lymph nodes. In human males, prostatic neoplasia is hormone-dependent and hormone therapies have been described. Canine prostatic neoplasia is not hormone-dependent; in fact, several studies have identified castration as a risk factor for development of prostatic neoplasia in dogs although the increased risk of development of prostatic neoplasia is not so great as to outweigh the benefits of castration. Prostatic neoplasia is the only disorder that can cause significant prostate enlargement in a castrated male dog.
Because disease has spread by the time of diagnosis, dogs with prostatic neoplasia may present with any number of clinical signs including lameness, fatigue, coughing, difficulty urinating or defecating, or weight loss. The prostate is asymmetrically enlarged and very firm on rectal palpation and the dog may be painful as it is compressed.
Prognosis with this disease is poor, requiring your veterinarian to do a definitive diagnostic test. Ultrasonography sliould be performed to permit accurate collection of an aspirate or biopsy specimen to be submitted to a pathologist.
Treatment is palliative. Anti-inflammatory medications may make the animal more comfortable. Surgical removal of the prostate, as is performed in humans, is associated with many post-surgical complications including urinary and fecal incontinence in dogs and so is not routinely performed.
Prostate disease is common in dogs and those of you with intact males definitely will have to deal with it at some point. While it has some similarity with human prostate disease, significant differences exist, too, making it dangerous to try to extrapolate your own experience onto your affected dog. Ongoing research will help us better diagnose and manage prostate disease in dogs in the future.
This article is reprinted on this site with permission from the author.
Breeder/Exhibitor Ed, Health
COMMON NAME
|
BOTANICAL NAME
|
POISONOUS PARTS
|
|
BIRD OF PARADISE
|
Strelizia regirae
|
FRUIT, SEEDS
|
|
BOSTON IVY
|
Parthenocissus quinquefolia
|
ALL PARTS
|
|
CALADIUM
|
Caladium
|
ALL PARTS
|
|
CREEPING CHARLIE
|
Glecoma hederacea
|
ALL PARTS
|
|
DUMBCANE
|
Dieffenbachia
|
ALL PARTS
|
|
EMERALD DUKE
|
Philodendron hastatum
|
ALL PARTS
|
|
GLACIER IVY
|
Hedera helix
|
LEAVES, BERRIES
|
|
MARBLE QUEEN
|
Scindapsus aureus
|
ALL PARTS
|
|
MAJESTY
|
Philodendron hastatum
|
ALL PARTS
|
|
NEPHTHYTIS
|
Synogonium
|
|
|
ARROWHEAD VINE
|
Podophyllum albolineatum
|
ALL PARTS
|
|
PARLOR IVY
|
Philodendron cordatum
|
ALL PARTS
|
|
POTHOS
|
Scindapsus aureus
|
ALL PARTS
|
|
RED PRINCESS
|
Philodendron hastatum
|
ALL PARTS
|
|
SADDLELEAF
|
Philodendron selloum
|
ALL PARTS
|
|
SPLIT LEAF
|
Philodendron Monstera deliciosa
|
ALL PARTS
|
|
UMBRELLA PLANT
|
Cyperus alternifolius
|
ALL PARTS
|
POISONOUS OUTDOOR PLANTS
COMMON NAME
|
BOTANICAL NAME
|
POISONOUS PART
|
| APRICOT |
Prunus ameniaca |
STEM, BARK, SEEDS |
| AZALEA |
Rhododendron occidentale |
ALL PARTS |
| BANEBERRY |
Actaea spicata |
BERRIES, ROOTS, LEAVES |
| BUCHBERRY |
Lantana |
ALL PARTS |
| CASTOR BEAN |
Ricinus communis |
SEEDS, IF CHEWED |
| CHOKE CHERRY |
Prunus virginica |
LEAVES, SEED PITS, STEM, BARK |
| DAFFODIL |
Narcissus |
BULBS |
| DAPHNE |
Daphne mezereum |
BERRIES, BARK, LEAVES |
| FOXGLOVE |
Digitalis purpura |
LEAVES, SEEDS, FLOWERS |
| HEMLOCK |
Conium maculatum |
ALL PARTS |
| HENS-AND-CHICKS |
Lantana |
ALL PARTS |
| HYACINTH |
Hyacinthus orientalis |
BULBS, LEAVES, FLOWERS |
| HYDRANGEA |
Hydrangea macrophylla |
LEAVES, BUDS |
| JERUSALEM CHERRY |
Solanim pseudocapscium |
ALL PARTS |
| JIMSON WEED |
Datura stramonium |
ALL PARTS, UNRIPE FRUIT |
| JONQUIL |
Narcissus |
BULBS |
| LILY-OF-THE-VALLEY |
Cornvallaria majalis |
ALL PARTS |
| MANDRAKE |
Podophyllum peltatum |
ROOTS, FOLIAGE, UNRIPE FRUIT |
| MISTLETOE |
Phoradendron flavenscens |
BERRIES |
| MORNING GLORY |
Ipomoea violaces |
SEEDS |
| NIGHTSHADE |
Atropa belladonna |
ALL PARTS |
| OLEANDER |
Norium oleander |
ALL PARTS, INCLUDING DRY LEAF |
| POINSETTIA |
Euphorbia pulcherrima |
LEAVES, FLOWERS |
| POKEWEED, INKBERRY |
Phytolacca americana |
ALL PARTS |
| RED SAGE |
Lantana camara |
GREEN BERRIES |
| RHODODENDRON |
Rhododendron |
ALL PARTS |
| RHUBARB |
Rheum raponticum |
LEAVES |
| SWEET PEA |
Lathyrus odoratus |
SEEDS, PODS |
| TULIP |
Tulipa |
BULBS |
| WISTERIA |
Wisteria |
SEEDS, PODS |
| YEW |
Taxus |
NEEDLES, BARK, SEEDS |
Breeder/Exhibitor Ed, Health
Breeder/Exhibitor Ed, Health
Commonly referred to as “Pano” by breeders, this mysterious disease/disorder occurs when the normal process of bone degeneration and resorption fails to happen. As a result, there is an excess formation and thickening of bone, which commonly affects the long bones of either the front legs (humerous) or hind (femur or tibia) legs.
Panosteitis is thought to be a disease of the osteoblasts. Osteoblasts are the cells within the bone that form the tissue and minerals that give bones their strength. Pan (generalized)- os (of certain bones) – itis (inflammation). Therefore it is described as a generalized inflammation of certain bones, specifically it occurs in five of the long bones – the humerous, radius, and ulna of the foreleg, and the femur and tibia of the hind leg.
Males are reported to be of higher risk than females for panosteitis. There is a nearly 4:1 ratio of males to females affected by panosteitis with the clinical signs being more severe and the disease/disorder more nearly chronic in males.
Symptoms are usually a sudden intermittent lameness which may last a few days to several weeks and then shift to a different leg. The lameness may be mild to moderate and seems to be unaffected or unchanged by rest or exercise. Lethargy and loss of appetite may also occur. Typically it usually is seen first in a foreleg.
Diagnosis is usually done by a vet by pinching the middle of the shaft of the affected suspected bone. If a definite pain response if gotten, it is usually panosteitis. If the pain is at the distal end of the long bone, it could be HOD instead.
Age of onset is usually between 4 to 18 months of age.
Causes : although the cause is still unknown, it is thought by some that dogs that are fed a “rich” high protein diet are the ones that will come up lame first. Some breeds appear to be predisposed to panosteitis and those are large breeds where their growing occurs very quickly during the first year. It has been suggested that changing to a lower protein but still highly- digestible food has stopped the course of panosteitis. Growth rate is a possible factor. Interestingly enough, whenever vaccines, flea powder, worm medicine, diet and other environmental factors have been indicated, the common denominator was found to be physiological stress.
Panosteitis is a self-limiting disease meaning that it will “go away” whether it is treated or not.
It occurs only in dogs. Even though cause is unknown, it has been reported that high protein diets may make the symptoms worse and last longer.
Breeder/Exhibitor Ed, Health
Breeder/Exhibitor Ed, Health